An Overview of Primary Hyperoxaluria Type 1
Primary hyperoxaluria type 1 (PH1) is a rare, progressive, inherited metabolic stone disease that is potentially life-threatening, and often presents with kidney stones.1-3
PH1 IS A RARE, PROGRESSIVE, INHERITED METABOLIC STONE DISEASE1-3
Primary hyperoxaluria (PH) is a group of autosomal-recessive metabolic stone diseases resulting from defects in different enzymes involved in glyoxylate metabolism that lead to an overproduction of oxalate in the liver.2,3 There are 3 types of PH: PH1, PH2, and PH3, each of which is caused by a defect in a different enzyme.3
PH1 often presents with kidney stones and is caused by autosomal recessive mutations in the AGXT gene, which impairs the function of the liver-specific enzyme alanine:glyoxylate aminotransferase (AGT).1,3 Normally, AGT processes glyoxylate, which is generated by another liver enzyme, glycolate oxidase (GO).2,3
Early Diagnosis is Critical2-6
PH1 is progressive and systemic2,9
See how PH1 can be life-threatening2
PH1 leads to progressive decline in kidney function.2
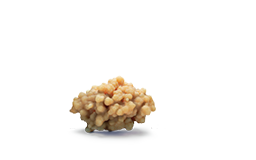
EXCESS OXALATE CAN DAMAGE THE KIDNEYS9
Liver oxalate overproduction may lead to inflammation and progressive kidney function decline following calcium oxalate crystal formation.9 Continuous oxalate overproduction may lead to irreversible damage in the kidneys and other organs.9
PH1 advances at variable rates, progressing to ESKD.2 When the kidneys are unable to excrete oxalate effectively due to toxicity from calcium oxalate crystal deposition, systemic oxalosis—the widespread tissue deposition of calcium oxalate—can occur.9 Complications from systemic oxalosis can be fatal.2
In some instances, kidney function can decline after a single incident of dehydration due to acute illness or intense physical activity.10-14 This can occur even in patients with previously stable disease.11
What causes oxalate overproduction in PH1?
Inability of AGT to process glyoxylate made by GO2
PH1 is a genetic disease caused by mutations in the AGXT gene that renders the liver enzyme AGT dysfunctional.3
Normally, AGT processes glyoxylate, which is generated by another liver enzyme, GO.2,3 In PH1, a defect in AGT means glyoxylate is instead converted to oxalate.2 Oxalate cannot be metabolized and is typically excreted by the kidneys at normal levels.3 When overproduced as it is in PH1, oxalate can wreak progressive, irreversible damage.2 Oxalate combines with calcium, creating calcium oxalate crystals.2 These crystals attach to kidney tissues, where they can aggregate to form kidney stones or lead to nephrocalcinosis.2,9 As calcium oxalate accumulates, kidney excretion is impaired, and crystals deposit throughout the body.9

"Given the nature of this disease, PH1 can go undiagnosed for many years. Early symptoms in adults, such as kidney stones, are often attributed to other, much more common conditions. We need to help physicians recognize symptoms faster, to potentially stop progression before a patient reaches end-stage renal failure."