KNOW THE SIGNS OF PH1
Primary hyperoxaluria type 1 (PH1) has heterogeneous clinical manifestations.1 However, if you know what to look for, working towards a diagnosis can be straightforward.2,3
RECOGNIZING THE SIGNS AND SYMPTOMS OF PH1*
PH1 is a heterogeneous disease.1,4 PH1 patients with identical genotypes, and even members of the same family, can have variable disease symptoms.4 At any age, patients may present with one or more of the clinical manifestations below1,5:
*These are not all the possible signs, symptoms, or complications of PH1, and not all patients exhibit them at the same time.
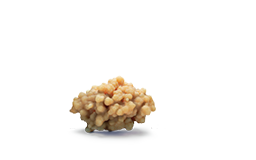
Kidney stones are the most common clinical manifestation and the one that most often leads to a diagnosis of PH1, though not all patients with PH1 may be stone formers.5,8,9 Metabolic testing through 24-hour urine collection analysis is recommended by the American Urological Association (AUA) in high-risk and recurrent stone formers.10
In a study, children with PH1 were characterized by presentation before adolescence, normal mobility, nephrocalcinosis, decreased eGFR, and calcium oxalate monohydrate stone composition†‡§—awareness of these characteristics could help with earlier diagnosis, which is crucial given the progressive nature of the disease.11
†Compared to controls of children with kidney stones not caused by PH1 in a study conducted using the PEDSnet database, a clinical research network of 8 US academic pediatric health systems, including 37 patients with PH1 and 147 controls (clinical characteristics of the PH1 group vs the control group that were statistically significant [P<0.05]).11
‡The case-control study of patients <21 years of age used electronic health record data collected between 2009 and 2021 from 8 US health systems.11
§Most control patients did not have genetic testing; urine chemistries were not performed on all patients; diagnostic coding errors may exclude some patients with PH1.11
REGARDLESS OF KIDNEY FUNCTION, ACUTE DECLINE CAN OCCUR SUDDENLY12,13
Though the course of PH1 is well characterized, with patients typically advancing toward ESKD, the rate of progression is variable.1,5,14 In some instances, kidney function can decline after a single incident of dehydration due to acute illness or intense physical activity.12,13,15-17 This can occur even in patients with previously stable disease.15
PH1 can be potentially life-threatening, often due to complications of ESKD and/or systemic oxalosis1,5
Once the estimated glomerular filtration rate declines to below 30-45 mL/min/1.73 m2, systemic oxalosis can occur because the kidney is unable to excrete oxalate effectively due to excess accumulation of calcium oxalate crystals.5,7
Diagnose as soon as possible to ensure prompt management.1-3,7,20,21
AUA PH1 RECOMMENDATIONS
The AUA recommends genetic testing to help confirm a PH1 diagnosis in any patient with urinary oxalate (UOx) excretion exceeding 75 mg/day (0.83 mmol/1.73 m2/day).‖10 Genetic testing can identify AGXT gene mutations to help confirm a PH1 diagnosis, regardless of kidney function.3,22
‖In adults without bowel dysfunction.

"On the outside, everybody looks normal. They act normal…but everything with PH1 is really internal, and it's what's going on inside, which most people don't know, and most people don't recognize."
Kidney stones may be a sign of something more serious6
Recurrent and/or unusual kidney stones in an adult or any kidney stone in a child or adolescent could be a sign of a metabolic stone disease like PH1.6,23 Consider these patients for a full work-up and genetic testing to help confirm PH1.6